Background: Venous thromboembolism (VTE) is a recognized complication of sickle cell disease (SCD). SCD confers a life-time risk of development of VTE, with a cumulative incidence of 11.3% by age of 40 years based on Cooperative group studies. Patients with SCD and VTE have a higher mortality rate (HR, 2.32; 95% CI, 1.20-4.46) compared to those without VTE (Naik et al, Am J Med. 2013;126(5):443-449). However, it remains unclear if this thrombotic pre-disposition improves after allogeneic hematopoietic stem cell transplantation (allo-HSCT).
Methods: This is a retrospective single institution cohort study of SCD patients with history of VTE and/or cerebrovascular accident (CVA) who underwent allo-HSCT for indications of CVA, recurrent acute chest, or organ dysfunction related to SCD. Inclusion criteria included SCD genotype, VTE of any location, or CVA confirmed on ultrasound, V/Q scan, or CT/MRI angiography/venography. The number and proportion of VTE and CVA events were recorded before and after allo-HSCT. Patients who had VTE events prior to transplant did not have their anticoagulation or aspirin continued post-transplant. Statistical and clinically significant differences were identified using non-parametric analysis using McNemar's method with exact probability and binomial distribution. Multivariate analysis was done to identify potential explanatory variables within results.
Results: 26 patients with SCD met inclusion criteria, all had HbSS genotype. 23 patients (88%) underwent HLA-haploidentical bone marrow transplant (haplo-BMT) with reduced intensity conditioning and 3 (12%) patients had myeloablative matched sibling donor transplants (MSD). Graft-versus-Host Disease (GVHD) prophylaxis included posttransplant cyclophosphamide/sirolimus/mycophenolate and cyclosporine/methotrexate in haplo-BMT and MSD, respectively. All patients had standard infection prophylaxis. The median age was 25 years (range: 8-54) at transplant and 17 patients were male (62%). 18 patients were taking hydroxyurea and 9 were on chronic transfusion therapy. Two patients had a second transplant for prior graft failure following haplo-BMT, all achieved 100% donor chimerism on days 30 and 100.
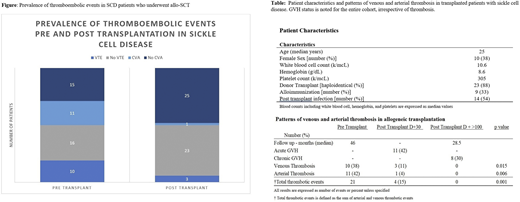
Median follow up for the cohort was 74.5 (range:10-212) months total and 28.5 (range: 9-111) post allo-HSCT. Prior to allo-HSCT, 10 patients developed 7 deep vein thrombosis (DVT) and 3 pulmonary emboli. Seven of these (70%) were unprovoked events. 11 patients (40%) had ischemic CVA. Post-transplant, there were two provoked DVTs and one embolic stroke events in three patients, of which two had a history of provoked VTE (Figure). One DVT and the embolic stroke were associated with venous catheter use in a patient with PFO (patent foramen ovale). Only one patient had grade two acute GVHD after development of DVT. All events occurred within 30 days post transplantation and during acute hospitalization. No further VTE occurred after 3 months of anticoagulation in all patients.
There was an absolute difference of 25% [95% CI=4.87- 26.9, p=0.015] in the prevalence of VTE events before and after allo-HSCT. In addition, there was an absolute 38.5% [95% CI=10.63-45.96, p=0.006] difference in the number of ischemic CVA before and after allo-HSCT. GVHD status, infection rates, age, history of pulmonary hypertension, and gender did not reach significance in explaining variation in results on logistic multivariate analysis (p > 0.05).
Conclusion: In patients with SCD with a history of thrombosis, there is an observed reduction in prevalence of VTE and stroke events post transplantation. Allogeneic stem cell transplantation may attenuate the ongoing activation of the coagulation cascade and hypercoagulable state in SCD. This needs to be validated in a larger prospective cohort study.
Green:Scripps: Honoraria, Other: travel; North American Thrombosis: Honoraria; CSL: Research Funding; Baxter,: Research Funding; Baxalta: Research Funding; Shire US Inc: Other: clinical trial support. Dholaria:bms: Research Funding; Poseida: Research Funding; Angiocrine: Research Funding; Takeda: Research Funding; J&J: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal